What is stress?
Stress starts in the brain, with a thought. Whether a real or perceived threat to our survival, or a positive uplifting exciting moment, our brain then initiates a sequence of steps that release hormones into our blood stream to ultimately make the body do something. As such stress can be positive or negative in its outcome. A positive stressor is something as simple as getting out of bed in the morning. If our cortisol didn’t rise in levels then we would find it very difficult to get moving. However, the body can also overreact to stressors that are not life-threatening, such as traffic jams, work pressure, and family difficulties. Instead of then dialing down the response, we can find ourselves in a state of long term ‘ready to run’ or standby mode. Chronic activation of this survival mechanism impairs health. Surges of stress hormones on a constant basis damage blood vessels and impact the way our body burns carbohydrates and stores fat.
Where does menopause come into the whole brain thing?
In all brains Oestradiol has multiple effects on brain function. Oestradiol can pass the blood-brain barrier and in addition the brain can create an internal supply of its own from cholesterol. Oestradiol is a critical signalling molecule within the brain and also protects the brain from the effects of aging.
[NB. Oestrogens are not made solely in the ovaries, are not exclusive to women and therefore the function of Oestrogens in the brain should be of interest to everyone.]
In women the brain and ovaries are part of the neuro-endocrine system. The health of the ovaries is linked to the brain and vice versa. Oestradiol is part of the signalling pathway that creates a conversation between the brain and the ovaries, every single day during our reproductive years. Oestradiol is key to energy production inside the brain. When it is high, brain energy is high. When it declines, brain cells slow down. We can feel this hormonal sensation happening long before we notice the physical effects, not just during perimenopause but also at times of other hormonal shifts such as menstruation and pregnancy. During the transition toward menopause total oestradiol levels decline erratically due to unpredictable changes in ovarian activity. Hot flushes, night sweats, insomnia, memory loss, mood swings, depression and anxiety are neurological symptoms of menopause.
However, postmenopause we no longer have the same level of neuro-protection and postmenopausal women are at an increased risk of developing brain conditions such as depression and dementia.
“Sex hormones, particularly estrogens, possess potent antioxidant properties and play important roles in maintaining normal reproductive and non-reproductive functions. They exert neuroprotective actions and their loss during aging and natural or surgical menopause is associated with mitochondrial dysfunction, neuroinflammation, synaptic decline, cognitive impairment and increased risk of age-related disorders. Moreover, loss of sex hormones has been suggested to promote an accelerated aging phenotype eventually leading to the development of brain hypometabolism, a feature often observed in menopausal women and prodromal Alzheimer’s disease (AD)” – article here
Here’s a reminder of the hormonal decline blueprint showing the fluctuating and downward decline of oestradiol.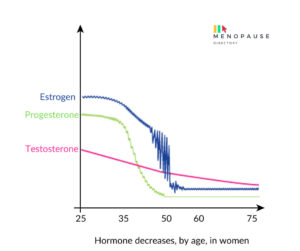
The cortisol connection –
During this life-long story and strong relationship between the brain and oestradiol there is an antagonist, namely cortisol, one of the hormones associated with our stress response. High cortisol levels have an impact on the effectiveness of oestradiol in the brain. In other words, if you want the oestradiol you do have to perform at its best in your brain, you need to manage your stress levels as much as possible to keep cortisol levels at optimal amounts. This is why your ability to manage situations you once thought of as not that stressful, may now tip the balance. As such those neurological symptoms of perimenopause – Hot flushes, night sweats, insomnia, memory loss, mood swings, depression and anxiety – will ebb and flow not only because of the fluctuating levels of oestradiol but because of constantly changing levels of cortisol.
Let’s look at an example of a potentially low performing oestradiol moment in relation to your menstrual cycle –
Example 1 – Cortisol high because cat was sick, kids screaming, computer crashed. Day 1 of your cycle so Oestradiol is low and you just started a crime scene heavy period.
Oestradiol’s normal anti-inflammatory job is now being trodden on from a great height by the cortisol and the fact it’s low in levels anyway at this point in the month. It would be fair to say at this precise moment in time your stress management potential is highly nobbled. What happens next if the kettle breaks? It’s not a life or death situation at the end of the day, but does it become a ‘straw that broke the camel’s back’ moment?
Example 2 – If the same high cortisol events had occurred on a day two weeks later on Day 14, when Oestradiol is high, not only would the kettle breaking not bother you, but you’d easily prepare a 3 course meal for a group of work colleagues at the drop of a hat Ready, Steady Cook style, and probably have enough energy left over the next day to complete the year 6 Egyptian Mummy project.
Now let’s throw in perimenopause …
Example 3 – same high cortisol, but absolutely no idea how you are likely to respond to a stressful situation and you have no idea where you are on your menstrual cycle because your periods are so irregular and your oestradiol is up and down like a yo yo!
In summary: High cortisol levels have an impact on the effectiveness of oestradiol in the brain. In other words, if you want the oestradiol you do have to perform at its best in your brain, you need to manage your stress levels as much as possible to keep cortisol levels at optimal amounts.
What are you doing to reduce cortisol and maintain a healthy brain during perimenopause?
Cortisol is like a built in alarm system that prepares you for running away from lions and tigers, but has probably been on a repeat snooze due to constant over stimulation. What stressors are you up against that may have left your snooze button on repeat and elevated the background levels of cortisol? What steps can you take to control your cortisol on a daily basis and therefore maximise the efficiency of your oestradiol in the brain?

