The silent long-term consequence of menopause
For many women, menopause is about more than just hot flashes and disappearing periods. Even though it signals the end of a woman’s reproductive years, menopause can also change the body in ways that might seem less obviously related to hormones.
One of these sometimes unexpected—but still related—issues is osteoporosis, a disease that weakens bones increasing your risk of fractures. Osteoporosis can progress quietly without any symptoms or pain until sudden breaks occur, usually in the back and hips. Menopause and just after menopause is a time when osteoporosis commonly presents itself, so it is important to be aware of the facts!
Bone is a living tissue that constantly renews to keep itself strong. Oestrogen is an important part of this process. Until around age 30, we normally build more healthy bone than we lose, but after our 30’s, bone tissue naturally starts to decrease. With age and reduced Oestrogen levels, particularly when the menopause occurs before the age of 45, there is an increased risk of progressive loss of bone density leading to bone thinning and fragility (Osteoporosis). Although bone loss occurs in both women and men, the loss is more rapid and is more common in women.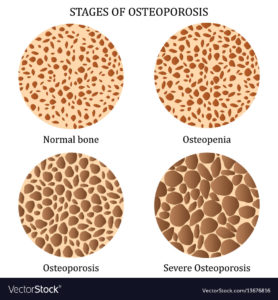
Bone thinning itself does not cause any symptoms, with Osteoporosis being known as the “silent disease”. (The aches, pains and stiffness many women experience around menopause, whilst caused by lack of oestrogen, are not the bones themselves aching, but the joints ligaments and other structures close to bones). The first warning sign of Osteoporosis can be a fracture after a simple fall or bump. A hump to the upper back is a common sign in longstanding Osteoporosis as deformity from weak bones occurs, and height is lost. It is estimated that by the age of 70 one third to one half of women will have had an Osteoporosis related fracture. Fractures commonly occur in the wrist, spine and hip. Such fractures can significantly reduce quality of life, independence and, in the case of hip fracture, can shorten life.
It is estimated that by the age of 70 one third to one half of women will have had an Osteoporosis related fracture. Fractures commonly occur in the wrist, spine and hip. Such fractures can significantly reduce quality of life, independence and, in the case of hip fracture, can shorten life.
Development of Osteoporosis in women is influenced by the strength of their bones before menopause: peak bone mass is achieved in our twenties and is influenced by weight bearing exercise, diet, adequate intake of calcium and vitamin D and by genetic influences.
Risk factors for osteoporosis include:
- Breaking a bone after a simple fall or bump
- Premature (before age 40) or early (before age 45) menopause
- Family history of osteoporosis
- Maternal history of hip fracture
- Long term (more than 3 months) or high dose use of steroids
- Smoking
- Excess alcohol intake
- Poor dietary intake of calcium
- Lack of weight bearing exercise
- Lack of sunlight – vitamin D deficiency
General factors which can therefore help to reduce the risk of osteoporosis include:
» Adequate sun exposure(vitamin D) is vital for Calcium absorption: In the UK, from March to September most people can get sufficient vitamin D from safe, daily sun exposure. However, between October and March, the NHS recommends that adults consider taking a daily 10mcg supplement of vitamin D.
» A healthy, varied, well balanced diet which is rich in calcium, e.g. from dairy products, green leafy vegetables and oily fish. Check dietary Calcium intake is sufficient with this easy to use calculator here
» Not smoking
» Limit alcohol intake (keeping below 14 units per week)
» Avoid excess caffeine by limiting tea / coffee / fizzy drinks
» Take regular weight bearing exercise, such as walking
» HRT can help to prevent Osteoporosis and reduce the risk of fracture. It is particularly important for women who have had an early menopause to consider using HRT, even if they haven’t got menopause symptoms so their bone health can be maintained.

